Findings
Please see COVIDProtocols.org, The Harvard Medical School Library of Evidence, and this resource from Radiopedia.
Typical Appearance: Mimics organizing pneumonia.
-
- Distribution is typically bilateral, peripheral, and basal predominant. Ground-glass opacities with or without consolidation
- Reverse-halo sign is present in a large minority (Simpson, RSNA, 2020)
- Bilateral findings in about 85% of patients; 33 – 86% predominantly peripheral and 70 – 80% predominantly posterior (Chung, RSNA, 2020; Song, RSNA, 2020)
- “Crazy paving” often develops later in the course of disease
Chest CT – Typical
78-year-old woman
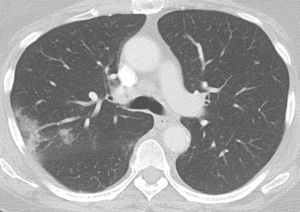
Note peripheral opacity with reverse halo sign


And other more nodular opacity
Hammer, Chest Observatory Boston
Indeterminate Appearance: Nonspecific
-
- Multifocal, perihilar or unilateral GGO with or without consolidation, lacking specific distribution, non-rounded or non-periphera
- Few, very small GGO, non-rounded and non-peripheral
Atypical Appearance
-
- Isolated lobar or segmental consolidation without GGO
- Discrete small nodules (centrilobular, “tree-in-bud”)
- Cavitation
- Smooth interlobular septal thickening with pleural effusions
Parenchymal imaging findings are variable and depend on timecourse (Wang, RSNA, 2020):
-
- Days 0-5: ~65% pure GGOs, 24% GGOs with intralobular lines
- Days 6-11: ~40% pure GGOs, 22% pure GGO with intralobular lines, 28% GGO with irregular lines and interfaces
- Days 12 – 17: more consolidations (38% show “mixed” pattern of consolidation, GGOs, and reticular opacities with architectural distortion)
- Late findings may include architectural distortion
- Small bilateral effusions can be seen in <10% of patients; large effusions are not typical.
- Large effusions, cavitations, discrete nodules, lymphadenopathy suggestive of another process (eg superimposed bacterial infection)
Portable CXR: Sufficient in most cases.
- Avoid routine daily CXR (unlikely to change management, evaluate case-by-case).
- May be initially normal in up to ~30% of hospitalized COVID patients, particularly in early disease (Wong, Radiology, 2019). Sensitivity 59% in one study, as compared to 86% for CT scan (Guan, NEJM, 2020)
CT Chest: Routine Screening CT for diagnosis or exclusion is not currently recommended. (Simpson, RSNA, 2020).
- CT will often will not change management and is associated with potentially unnecessary risk (risk to staff of transmission in transit, risk to patient for desaturation in transit).
- Avoid unless otherwise indicated: e.g. for abscess or empyema, or other causes of hypoxemia like pulmonary embolism
- Approximately 50% of CT scans are normal up to 2 days after symptom onset
Point of Care Ultrasound: Can be used by experienced providers,but is operator-dependent (Mayo, Intensive Care Med, 2019).
- Findings: Focal or diffuse B lines with sparing of uninvolved areas, irregular thickened pleural line with “scattered discontinuities”, subpleural consolidations (relatively avascular on Doppler), alveolar consolidations with air bronchograms
- May help distinguish cardiogenic pulmonary edema from ARDS. (Mayo, Intensive Care Med, 2019).
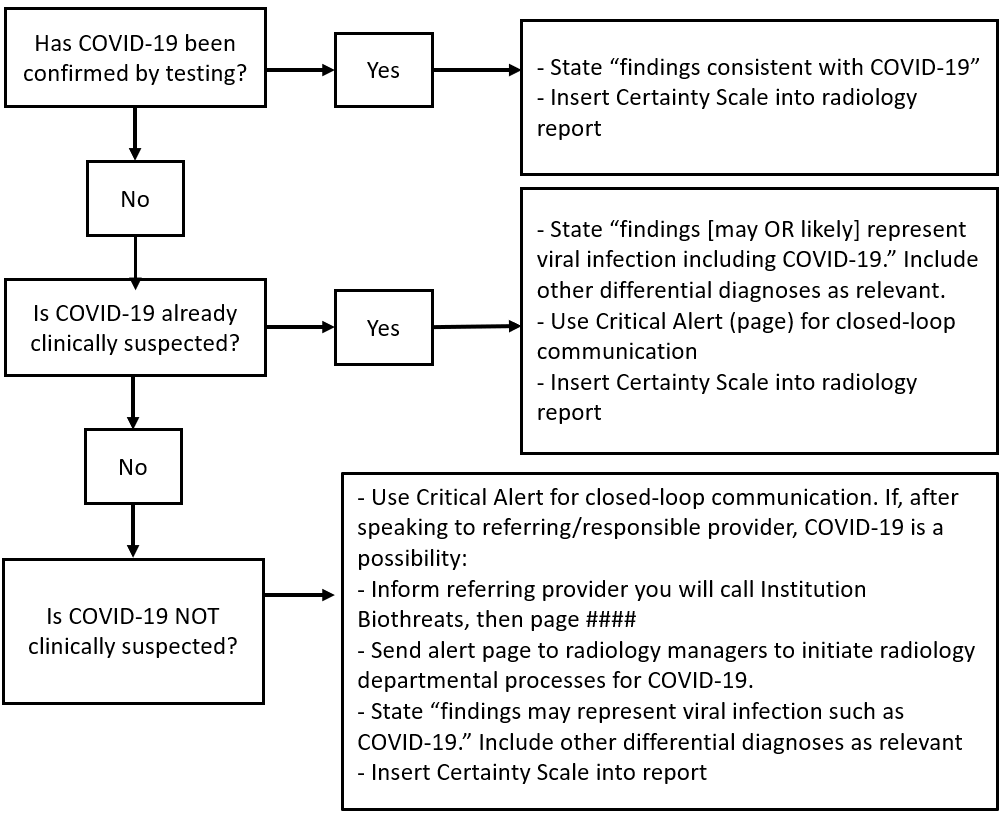
For Radiologists
Radiology Reporting Guidelines
Thoracic Imaging
- Impression: Typical findings of COVID-19
-
- If COVID-19 is already confirmed
- State that findings are “consistent with COVID-19”.
- Insert Certainty Scale at the bottom the report (powerscribe shortcut is type cs and press enter). (Hammer, JACR, 2020)
- If COVID-19 is clinically suspected
- State findings “may represent viral infection such as COVID-19”. Remember to include any other differential diagnoses, as appropriate, again using certainty terms.
- Use Orange ANCR (page) alert for closed loop communication with responsible or ordering provider.
- Insert Certainty Scale at the bottom the report (powerscribe shortcut is type cs and press enter). (Hammer, JACR, 2020Suggested additional Reporting Language: “Commonly reported imaging features of (COVID-19) pneumonia are present. Other processes such as influenza pneumonia and organizing pneumonia, as can be seen with drug toxicity and connective tissue disease, can cause a similar imaging pattern.” (Simpson, RSNA, 2020)
- If COVID-19 is clinically unsuspected
- Use Red ANCR (page) for closed loop communication with responsible or ordering provider. If after discussion with ordering/responsible provider COVID-19 becomes a possible diagnosis, you should mention COVID-19 specifically in your report using relevant certainty terms.
- Inform referring provider that you will contact Brigham Biothreats by paging 30331. This will initiate actions required by PHS/BH policy for COVID-19.
- Send purple alert page (or page) to Tyler Martin or Patrick Curley to initiate necessary radiology departmental processes for COVID-19.
- State findings “may represent viral infection such as COVID-19” (Hammer JACR 2020). Remember to include other clinically relevant differential diagnoses in your impression.
- Suggested additional Reporting Language: “Commonly reported imaging features of (COVID-19) pneumonia are present. Other processes such as influenza pneumonia and organizing pneumonia, as can be seen with drug toxicity and connective tissue disease, can cause a similar imaging pattern.” (Simpson, RSNA, 2020)
- Insert Certainty Scale at the bottom the report (powerscribe shortcut is type cs and press enter).
- If the imaging findings are that of a viral pneumonia but not typical for COVID-19, you simply report that “findings may/likely represent a viral pneumonia.”
- Suggested additional reporting language: “Imaging features can be seen with (COVID-19) pneumonia, though are nonspecific and can occur with a variety of infectious and noninfectious processes.” (Simpson, RSNA, 2020)
- If you have any questions about whether findings may represent COVID-19, you can consult thoracic radiology attending on call (or the reading room during the day). Consider using COVID-19 Consult option which has been set up in Worth Another Look (please page)
- DO NOT INCLUDE COVID-19 in your findings or impression other than scenarios 1-3 described above and be mindful that the absence of findings on imaging including Chest CT does not exclude COVID-19 infection. (Hammer, JACR, 2020)
- If COVID-19 is already confirmed
Cardiac Imaging
TTE
- Do not order routine TTEs on COVID-19 patients.
- Indications for POCUS:
- Marked elevation in troponin or NTproBNP or decline in ScvO2/MvO2
- Shock
- New heart failure (not pre-existing heart failure)
- New persistentarrhythmia
- Significant ECG changes
- If abnormalities are identified on POCUS (e.g. new reduction in LVEF < 50%), a formal TTE should be obtained and cardiology consulted. Where possible order limited TTEs instead of full TTEs to conserve resources.
Advanced CV Imaging (Stress Testing, TEE, CT, CTA, MRI, Invasive Coronary Angiography)
- All testing should be limited to cases where the information is thought to be critical to patient care. Consideration of all advanced imaging should be discussed with cardiology consultation or individual imaging teams.
- Stress testing is not expected to be commonly indicated in individuals with active COVID. If needed, consider pharmacologic nuclear stress testing or coronary CTA.
Specific Considerations During Acute COVID-19
TEE
- Only for absolute necessity
- Consider alternative noninvasive imaging modalities (e.g. cardiac CT to rule out left atrial appendage thrombus, cardiac CT and/or PET/CT for endocarditis complications).
Cardiac CT
- Consider for selected patients with elevated cardiac biomarkers with possible myocardial injury versus acute coronary syndrome. In this setting, the role of coronary CTA is to exclude obstructive CAD. At the same setting cardiac CT may also be used to evaluate left and right ventricular function. If needed, chest CT (to evaluate lungs) or pulmonary angiogram (to rule out PE) may be obtained in the same setting.
- Consider in selected patients as a substitute for TEE to rule out left atrial appendage or to evaluate for endocarditis.
Cardiac MRI
- Consider for selected patients with elevated cardiac biomarkers with possible myocarditis, if this information will impact patient management.
Nuclear Imaging
- In COVID patients who require stress testing, vasodilator stress testing is preferred over exercise testing.
Additional Specific Considerations for Imagers
Nuclear Imaging
- In selected patients who have recovered from COVID, PET MPI using a quantitative assessment of myocardial blood flow may be useful for evaluating for microvascular dysfunction.
Cardiac MRI
- In selected patients who have recovered from COVID, Cardiac MRI using Late gadolinium enhancement (LGE) may be useful for evaluating residual scar from myocarditis. In the acute and sub-acute periods, T1 and T2 mapping as well as assessment of extracellular volume fraction (ECV) may improve the sensitivity of detecting myocarditis. However, the prognostic significance of such abnormalities (especially in the presence of normal ventricular function or when LGE abnormalities are absent) is uncertain.
Cardiac CT
- For acute COVID patients, consider use of a multiphase data acquisition in order to evaluate left and right ventricular function.
- When clinically needed, a pulmonary CTA can be performed in the same setting to rule out the presence of a pulmonary embolus (PE). Such as scan would require a wider field of view and a higher contrast dose.
Echocardiography
- In acute COVID, evaluate for both left and right ventricular function.
- The differential diagnosis of abnormal right ventricular dysfunction include myocardial injury / myocarditis, hypoxemic vasoconstriction, pulmonary embolus, cytokine mediated. RV dilatation and RV dysfunction have both been shown to be associated with adverse prognosis.
- The differential diagnosis of abnormal left ventricular dysfunction include myocardial injury / myocarditis, acute coronary syndrome, and stress induced cardiomyopathy. In the setting of elevated cardiac troponin, the presence of regional wall motion abnormalities suggests the presence of an acute coronary syndrome; however, myocardial injury may also result in focal wall motion abnormalities.
REFRENCES:
| Publication | Year |
| Center for Evidence-Based Imaging | https://cebi.bwh.harvard.edu/signature-initiatives/covid-protocols-in-radiology/
|
| Harvard Medical School Library of Evidence | http://libraryofevidence.med.harvard.edu/app |
| Radiologist Reporting and Operational Management for Patients With Suspected COVID-19 | Hammer, Mark M. “Radiologist Reporting and Operational Management for Patients With Suspected COVID-19.” JACR (2020). https://www.jacr.org/article/S1546-1440(20)30645-1/pdf |
| Use of cardiac computed tomography amidst the COVID-19 pandemic – SCCT guidance document endorsed by ACC
|
Choi AD, Abbara S, Branch KR, et al. Society of Cardiovascular Computed Tomography guidance for use of cardiac computed tomography amidst the COVID-19 pandemic Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr 2020;14:101-4.
Living document: https://scct.org/page/COVID-19
|
| Safe Reintroduction of Cardiovascular Services During the COVID-19 Pandemic: From the North American Society Leadership 2 | Wood DA, Mahmud E, Thourani VH, et al. Safe Reintroduction of Cardiovascular Services during the COVID-19 Pandemic: Guidance from North American Society Leadership. J Am Coll Cardiol 2020. |
| Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic
Ramping Up Safely to a New Normal 1 |
Zoghbi WA, DiCarli MF, Blankstein R, et al. Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping Up Safely to a New Normal. JACC Cardiovasc Imaging 2020;13:1615-26. |
| Multimodality Imaging in Evaluation of Cardiovascular Complications in Patients With COVID-19 39
|
Rudski L, Januzzi JL, Rigolin VH, et al. Multimodality Imaging in Evaluation of Cardiovascular Complications in Patients With COVID-19: JACC Scientific Expert Panel. J Am Coll Cardiol 2020;76:1345-57.
|
| Management of Acute Myocardial Infarction During the COVID-19 Pandemic
|
Mahmud E, Dauerman HL, Welt FG, et al. Management of Acute Myocardial Infarction During the COVID-19 Pandemic. J Am Coll Cardiol 2020.
|
| ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic
|
Online at:
https://www.escardio.org/Education/COVID-19-and-Cardiology/ESCCOVID-19-Guidance (Last update: 10 June 2020)
|
| Society of Cardiovascular Magnetic Resonance Resources | https://scmr.org/page/COVID19
|
| Guidance and best practices for nuclear cardiology laboratories – Statement from ASNC and SNMMI | Skali, H., Murthy, V.L., Al-Mallah, M.H. et al. Guidance and best practices for nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: An Information Statement from ASNC and SNMMI. J. Nucl. Cardiol. 27, 1022–1029 (2020). https://doi.org/10.1007/s12350-020-02123-2
|
| American Society of Echocardiography COVID-19 Resources | https://www.asecho.org/covid-19-resources/
|